Introduction
The chest wall deformity program at the Bon secours Mercy Health, Children’s is one of our Signature Programs. Our program is a comprehensive Pediatric where we care for patients of all ages.
Recognizing that each patient’s needs are unique, we work with every child and his/her family to establish a customized treatment plan.
Our Multidisciplinary team
| Pediatric surgeons | Ashwin Pimpalwar, MD |
| Plastic surgeons | XYZ |
| Orthopedic surgeons | XYZ |
| Anesthesiologist | |
| Pulmonologist | |
| Radiologist | XYZ |
| Cardiologist | |
| Pain specialist | |
| Physiotherapist | |
| Physician assistants |
Conditions we treat
- Pectus Excavatum: Sunken/Funnel chest
- Pectus Carinatum: Protruding /Pigeon chest
- Mixed Deformities: Excavatum and Carinatum
- Poland syndrome: Chest wall muscle and ribs may be underdeveloped or absent
- Slipping ribs: The cartilage on the lower ribs slips and moves
- Congenital rib anomalies: Rib cartilage deformities
- Juene syndrome: Bell shaped Narrow chest
- Jarco levine syndrome: Crablike chest
Pectus Excavatum
Pectus excavatum, also known as sunken chest or funnel chest, occurs when an abnormal growth of cartilage within the chest wall pushes the sternum, or breastbone, and ribs inward, creating a caved-in or sunken appearance. Learn more about pectus excavatum.
Pectus Carinatum
Pectus carinatum, also known as pigeon chest, is when the cartilage grows up and out and forces the sternum forward. One or both sides of the chest can be affected. Learn more about pectus carinatum.
Diagnosis
Because of the visual nature of these conditions, pectus excavatum and pectus carinatum can usually be initially diagnosed by a physical examination of the chest wall.
Once the condition is diagnosed, your primary care physician may suggest you meet with a pediatric surgeon and their team to discuss treatment options.
At your Appointment?
Your first appointment will be a clinic consultation with an advanced practice nurse and a pediatric surgeon. A comprehensive past medical, surgical and family history will be taken at this visit, and a physical exam will also be completed. An in-depth description of the diagnosis and available treatment options will then be discussed.
After the initial visit, the surgeon may order a few tests to help build the treatment plan.
These are all outpatient tests and together their results will help define next steps. All patients will not necessarily have all tests.
Echocardiogram – this test is an ultrasound of the heart, which will assess for anatomy and function of heart.
Pulmonary Function Testing – this will tell the medical team the strength of the patient’s lung capacity. This test is completed in the Pulmonary Diagnostics lab.
CT/MRI Scan – depending on the age of the child and the severity of the condition, the surgeon may also order a CT scan of the chest. In addition to the white light scan, if needed, this test will be used to measure the precise severity and depth of the sunken chest.
Treatment of Pectus Excavatum & Pectus Carinatum
All of the test results will be reviewed to determine the best course of treatment. Both surgical and non-surgical options will be evaluated.
Pectus Excavatum
Pectus excavatum, also known as sunken chest or funnel chest, is the most frequent congenital anomaly of the chest wall, occurring in 1 in 400 births, and is found in 2.6 percent of children aged 7–14. It occurs when an abnormal growth of cartilage within the chest wall pushes the sternum, or breastbone, and ribs inward creating a caved-in or sunken appearance. If the ribs grow faster than the expansion of the heart and lungs, then the sternum can be pushed inward instead.
While it usually occurs as a stand-alone condition, up to 20 percent of patients may have other skeletal conditions, such as scoliosis.

Children Affected by Pectus Excavatum
The condition seems to be more common in boys than girls. It often doesn’t fully manifest until adolescence during rapid bone growth and if severe, can be treated with surgery at that time. The cause is not known, but there is sometimes a tendency to run in families.
Symptoms of Pectus Excavatum
It may cause children to sometimes feel shortness of breath or experience exercise intolerance or palpitations, interfering with heart and lung function. Regardless of the severity, as the child reaches the pre-teen or adolescent years, the caved-in or hollow appearance may make them self-conscious and can cause anxiety.
Diagnosis of Pectus Excavatum
Because of the visual nature of this condition, pectus excavatum can usually be initially diagnosed by physical examination of the chest wall. Depending on the symptoms and clinical findings, the medical team may request a series of tests including echocardiogram, pulmonary function test or CT scan.
Treatment of Pectus Excavatum
Although the initial care may include monitoring a patient’s growth and chest-specific physical therapy, surgical correction may be provided. The team will look at conservative treatment options, as well as surgery. Some other options may include physical therapy evaluation and treatment, as well as an annual follow-up in the Chest Wall Deformities Clinic.
If your child is an appropriate candidate for surgery, it is likely they will have either the minimally invasive Nuss procedure or rarely the open Ravitch procedure.
The Nuss procedure is a minimally invasive surgery. Incision sites are made on both sides of the chest wall and corrective, custom-fitted steel bar(s) are inserted under the sternum and secured in place. Typically these bar(s) remain in place for two to three years. The Nuss procedure, because of the smaller incisions, results in less obvious scarring.

Nuss Procedure: Before and after pictures


With the Ravitch procedure, the surgeon will make an incision to remove abnormal cartilage and place the sternum in the appropriate position. The surgeon may also insert a steel bar to support and elevate this area as it heals. When used, the bar is removed approximately two years later as an outpatient procedure. The Ravitch surgery is especially well suited for patients who do not wish to have a bar in place for more than one year and those with highly asymmetric chest wall deformities or problematic lower rib flaring.
The decision about which surgery is best for your child is based on a number of factors that are specific to each patient.
Non-surgical options
If the pectus excavatum is milder variety and does not fulfil the criteria for Nuss procedure or in patients who do not wish to undergo surgery, the option of Vacuum bell does exist.
Vacuum bell was made by German engineer Eckart Klobe. The Vacuum Bell uses a suction cup, creating a vacuum seal on the chest wall and lifts the sternum, thus correcting pectus excavatum through non-invasive treatment over time. The device allows patients to use it without interfering with school, sports and other daily activities.

Expectations Post surgery
Hospital Stay
For both the Nuss procedure and the Ravitch procedure, the average hospital stay is four to seven days.
Pain Management
The surgery for pectus excavatum is done under general anesthesia. Sometimes prior to surgery, an anesthesiologist may insert an epidural catheter into the back while your child is asleep. An epidural is a small tube that will allow your child to receive pain medication after surgery.
The teams at MU Children’s care very much about the comfort of patients after surgery and do everything possible to minimize any discomfort that can occur. After your child is awake and is in the recovery room, the recovery room nurse and the anesthesiologist work together to ensure that the child is as comfortable as possible.
Your child may receive a combination of Intravenous (IV) and oral pain medications after surgery. This may include the epidural or patient-controlled analgesia (PCA) pump.
Once your child is ready, the IV pain medications are stopped and your child will be transitioned to a combination of oral pain medications in preparation for discharge home. Most children will require two to three weeks of oral pain medications after they are discharged from the hospital.
Activity - Home
In terms of resuming normal activity, patients are generally advised to abstain from heavy physical exertion for about 6 weeks. This also means, no backpacks on the shoulder for three months so the area is not stressed.
They can return to very light aerobic activity, including walking and doing breathing exercises, 3 weeks after surgery. No running, working out, sit-ups or biking to protect the area.
After six weeks, patients can begin stronger cardiovascular conditioning such as running, swimming, biking or yoga.
After the initial six-week period of recovery, patients can slowly begin to engage in more intense sports, such as basketball or hockey. The operation is intended not to limit physical activity, but any reasonable precautions should be taken so as to avoid receiving a forcible blow to the chest, as that could cause the bar to shift.
Post-operative Follow-up
Routine post-surgical follow-up with your pediatric surgeon and team is important and should be done at regular intervals for up to two years post-surgery. Check with your surgeon on the exact interval timing.
Pectus Carinatum
Pectus carinatum, also known as pigeon chest, is when the cartilage grows up and out, which causes the sternum, or breastbone, to protrude out in front of the rest of the chest. One or both sides of the chest can be affected.

Children affected by Pectus Carinatum
This condition is less common than pectus excavatum. It seems to be more prevalent in boys than girls and is often most evident after a growth spurt when the child is in their pre-teen to early teenaged years.
Up to 50 percent of children with a pectus carinatum condition will have a close relative with a similar chest wall abnormality.
Symptoms of Pectus Carinatum
Most children with this condition do not experience symptoms, but for some, there may be chest pain during times of accelerated growth and development. Other children sometimes experience shortness of breath, especially when exercising. While the condition does not cause any known damage to the lungs or heart, psychological impact does affect the child’s body image and often self-esteem.
Diagnosis of Pectus Carinatum
Because of the visual nature of this condition, pectus carinatum can usually be initially diagnosed by physical examination of the chest wall. Depending on the symptoms and clinical findings, the medical team may request a series of tests including echocardiogram, pulmonary function test or CT scan.
Treatment of Pectus Carinatum
Although the initial care may include monitoring a patient’s growth, surgical correction may be provided. The team will look at conservative treatment options, as well as surgery. Some other options may include physical therapy evaluation and treatment, as well as an annual follow-up in the Chest Wall Deformities Clinic.
Non-Surgical Options (Dynamic compression Bracing)
Pectus carinatum may be effectively treated with conservative measures such as bracing or physical therapy. Various bracing option have been used in the past with non-optimal results. At our hospital we use the FMF Dynamic Compression Bracing. This is a custom-fitted, expandable, low profile, hypoallergenic, ultra-light aluminum brace designed to deliver the precise amount of pressure needed to gradually reshape the chest wall with minimal discomfort. The system was developed in Argentina and is being used worldwide.
At a child’s first consultation visit, we use a pressure-measuring device to measure the chest wall and determine how much pressure is needed to correct the pectus carinatum. We then take measurements of the chest wall for custom ordering the brace.
Once the brace arrives, we fit the brace for our patients and develop a treatment plan. We start with very low-pressure settings first and gradually increase the pressure at each subsequent visit.
Children return to the clinic once a month for an evaluation and adjustments. Once the pectus carinatum is corrected, the patient undergoes a weaning process till the brace is finally discontinued. This helps maintain the chest wall’s new shape.
Advantages of the FMF Dynamic Compressor


The major advantage of this bracing system is that it objectively measures the pressure needed to correct the condition. This measurement guides treatment decisions and helps the care team evaluate progress. It also allows the team to give an accurate prediction of how long treatment will last and what the chest wall will look like afterward. Also, results usually happen faster with this system compared to traditional bracing systems.
The success rate for the FMF Dynamic Compressor is greater than 90 percent when children or adolescents wear it as directed. Younger children and teens, who typically have a very soft and flexible chest wall, tend to do best. In the rare event the chest wall is too stiff and does not respond to bracing, surgery is still an option.
Surgical Options
For patients with pectus carinatum, surgery is not usually required. It is only considered if bracing is not effective, or if the patient is experiencing severe chest pain related to the abnormal growth of their chest wall.
If your child is an appropriate candidate for surgery, it is likely they will have the MIRPC (Minimally invasive repair of Pectus carinatum) or rarely the Ravitch procedure.
With MIRPC the patient will have the steel Bar placed subcutaneously to push the cartilages in to shape.

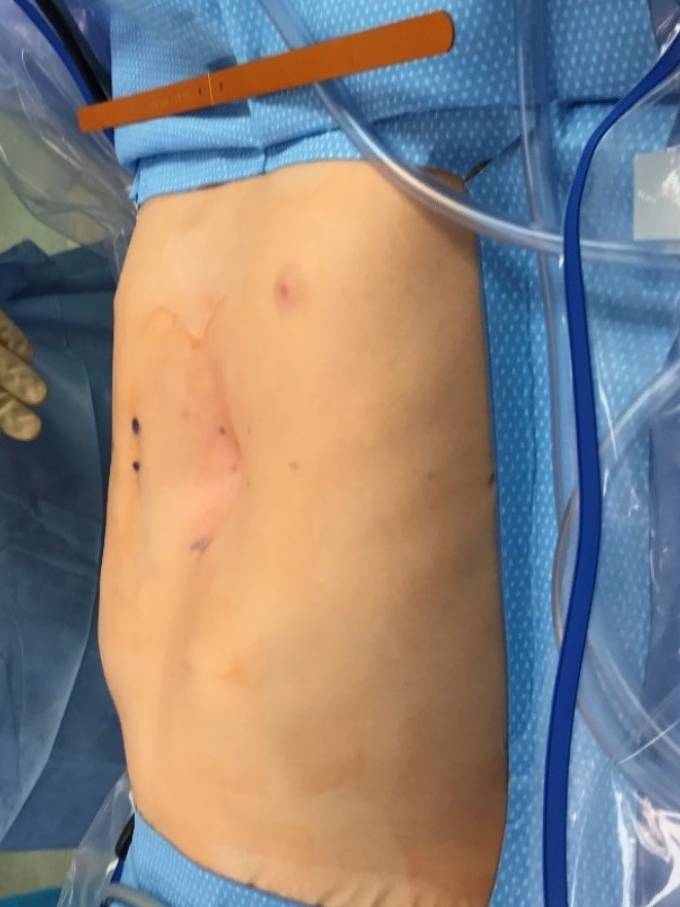
MIRPC for Pectus Carinatum: post correction picture.
With the Ravitch procedure, the surgeon will make an incision to remove abnormal cartilage and place the sternum in the appropriate position.
Post-surgical care
Hospital Stay
For the MIRPC and the Ravitch procedure, the average hospital stay is four to seven days.
Rest of the care is same as for Pectus excavatum patients.
Poland syndrome: Chest wall muscle and ribs may be underdeveloped or absent.

Why come to the Bon Secours Mercy Health, Children’s?
- Surgical expertise: Ashwin Pimpalwar, M.D. is a leader in the minimally invasive procedures used to treat some of the most complex chest wall deformities.
- Individualized care: Our surgeons take a whole-team approach to treating conditions. We work alongside specialists and subspecialists across our hospital, including cardiology, pulmonology, anesthesiology, pain management specialists and genetics, and are ready to meet a patient's needs all in one location.
- Minimally invasive approach to treatment: Our team is specially trained in minimally invasive procedures, such as the Nuss procedure, to repair some of the most complex deformities.
- Comprehensive pediatric care: We have access to pediatric specialists and subspecialists throughout our hospital and can provide a seamless transition for patients who need additional specialty care beyond our services.
- Long term outcomes excellent: Our team achieves a success rate that inspires families to travel hundreds of miles for care.